When Trauma Work Causes Harm: Recognizing OCD in Your Clients
Have you ever launched into trauma processing with a client, only to see their symptoms spiral? Many therapists are trained in trauma, fewer in OCD, but the overlap is common. When OCD is mistaken for trauma, well-intended interventions can reinforce the cycle.
OCD vs. Trauma: Why the Overlap Confuses Even Seasoned Clinicians
It is critical to understand the differences in the clinical presentation of OCD vs trauma. There is overlap in distress, avoidance of triggers, and hyperarousal. OCD can even get mislabeled as complex trauma. OCD can present like trauma, especially when compulsions look like “coping.”
Trauma Work Can Accidentally Harm Clients with OCD
How EMDR (and other trauma processing) can reinforce compulsions
EMDR without OCD stabilization can reinforce compulsions. ERP (Exposure and Response Prevention) is used to help clients increase their tolerance of uncertainty and distress. Combined with ACT (Acceptance and Commitment Therapy), clients learn how to spend their time and energy on activities aligned with their values and goals rather than performing compulsions. In this way, fear doesn’t need to be neutralized; it can be faced.
With exposure-centered trauma treatment, the client may work toward the goal of sensing safety and agency, so their nervous system can recognize that the traumatic experience is not currently threatening. Yes, both exposure approaches address discomfort head-on. The goals, expectations, and pacing are very different.
ERP + ACT vs. exposure-centered trauma treatment: similar tools, different aims
What marks success in trauma treatment and OCD look very different. For example, leaning into uncertainty with trauma work could exacerbate a lack of safety or activate the nervous system. Trauma-informed providers may offer reassurance to clients they believe are experiencing anxiety in an effort to offer stabilization, but what they actually do is send a client back through the OCD cycle because seeking reassurance is a compulsion that only provides temporary (not longer-term) relief.
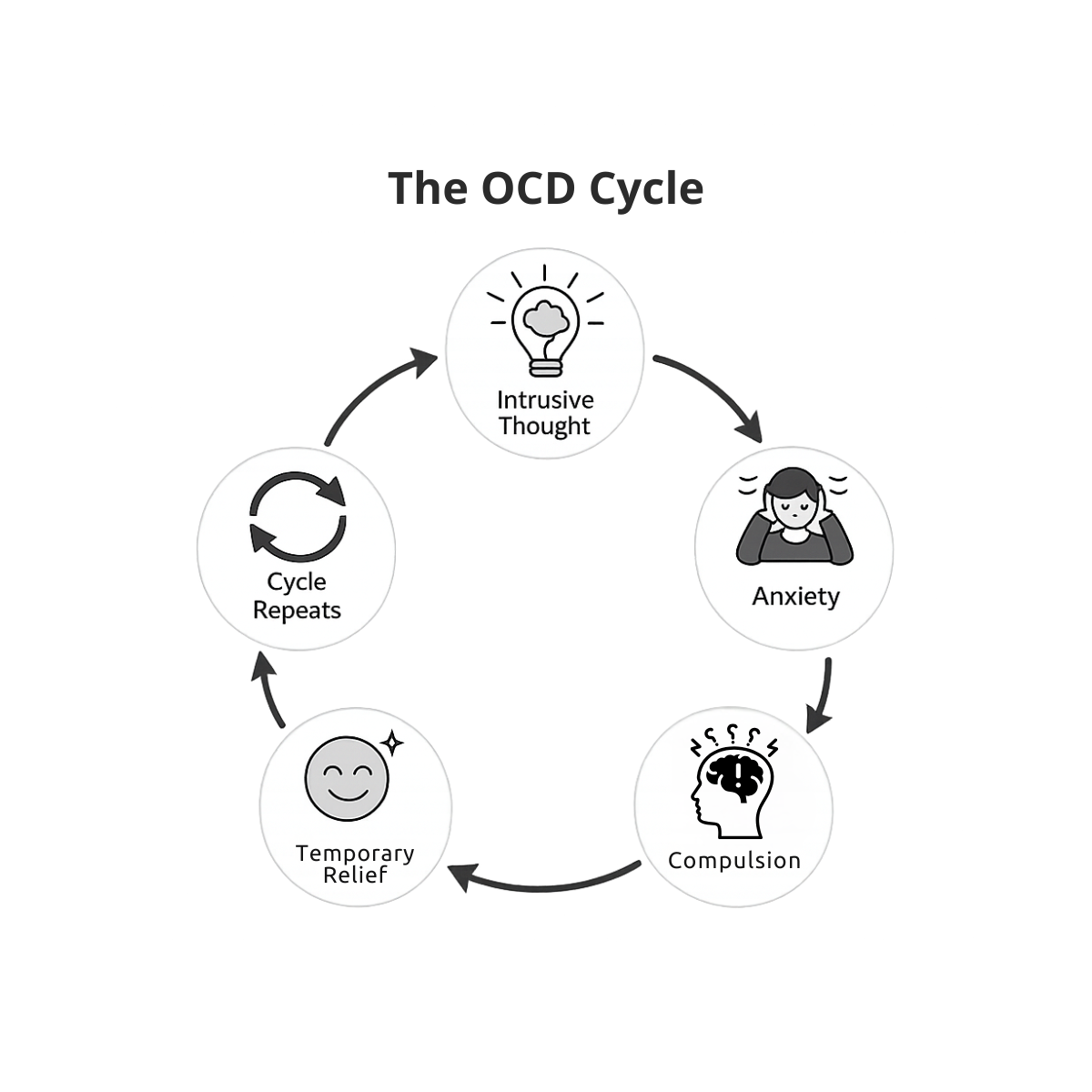
The OCD Cycle: Intrusive Thoughts, Anxiety, and Compulsions
Understanding the OCD cycle can help clinicians recognize when reassurance or “processing” may unintentionally function as a compulsion.
Clinical Red Flags: When “Processing” Might Be Part of the OCD Cycle
When treatment is not appropriately addressing OCD, a client may say things like:
“My intrusive thoughts got louder and more frequent after sessions.”
“I’m so glad we talked through that last time. I’d like to process more with you about that incident.”
“I’ve been monitoring/journaling/recording my thoughts constantly.”
“I felt calmer in session, but my rituals (like seeking reassurance) increased afterward.”
“I didn’t realize my coping skills had become compulsions.”
“You always make me feel better.”
In order to be more aware of the potential pitfalls here, take note if your client is repeatedly seeking reassurance in sessions. You may also notice “processing” or “talking through it” becomes ritualized, and they speak in excess about a scenario (or series of scenarios) without opportunity for a therapeutic interruption.
These are the times, though, for a healthy interruption—not to the conversation, but to the cycle. It is also possible that clients begin to use resources such as safe/calm state, repeating positive cognitions, and other grounding tools as compulsions.
Some elements of these behaviors that can tip you off if they are being used compulsively is if there is an emphasis on urgency, certainty, or full completion (black and white thinking).
What To Do Instead: Rule Out OCD, Refer, or Stabilize Before Reprocessing
In order to best serve your clients, ensure you understand the difference between anxiety and OCD and rule out OCD before continuing on to trauma work, such as EMDR. Refer clients with OCD to specialized clinicians equipped with evidence-based skills to support them. Alternatively, you could collaborate or consult with OCD specialists.
If you determine it is most appropriate for you to continue working with them, stabilize OCD symptoms before engaging in any reprocessing or other activating trauma work. Resourcing is key. Also, make sure your client understands the OCD cycle thoroughly so that they can identify when they are engaging in mental compulsions.
Ethics and Scope: Competence, Consultation, and Harm Reduction
There is harm in misapplied interventions. Our responsibility as clinicians is to know the limits of our competence and when it is time to refer out, consult, or expand our own knowledge base. Even seasoned trauma therapists can miss OCD.
Misapplied interventions can create harm, even with the best intentions. The goal isn’t to do less trauma work; it’s to do the right work in the right order. If you’re unsure whether OCD is complicating your case, consultation can help you clarify conceptualization, pacing, and next steps.
As an ASWB ACE provider and supervisor, I provide consultation for therapists navigating OCD/trauma overlap. If you’re working with a case where OCD and trauma are intertwined, and you want support clarifying next steps, consultation can help you move forward with more confidence and less risk of reinforcing the cycle. Click here to learn more.
Written by Kelsey Blahnik, LCSW-S
Kelsey Blahnik, LCSW-S, is an author, clinician, and advocate committed to bringing peace and justice into our politically divided world. With extensive experience in behavioral health, including work with substance abuse, unhoused individuals, and veterans, Kelsey has witnessed the impact of division on communities. She is the owner of a thriving online group therapy practice, The And Way Therapy, and author of the book The And Way: Assertive Peacemaking in a Divided World.
Outside the therapy room, you’ll usually find her reading, hiking, or enjoying matcha.
Schedule your professional consultation here.